Researchers at the University of Maryland School of Medicine (UMSOM) and Institute for Genome Sciences (IGS) have developed a groundbreaking method to create “digital twins” of cancer patients—computerized models that simulate how individual patients’ cells behave. Published in Cell on July 25, this work could transform how doctors predict treatment responses in cancer patients.
The innovation lies in a new plain-language “hypothesis grammar” that allows scientists to describe complex cell behaviors using simple English sentences. This grammar, developed by Dr. Paul Macklin at Indiana University, acts as a bridge between biology and computer models, enabling researchers to build detailed digital simulations of how diseases like cancer develop and respond to therapies.
Dr. Jeanette Johnson and Dr. Daniel Bergman of UMSOM used this approach to model how breast and pancreatic cancer cells interact with the immune system. By combining patient genomic data with spatial transcriptomics (which maps gene activity within tissues), they created simulations showing why certain cancers resist immunotherapy. For example, in pancreatic cancer, dense networks of fibroblasts (non-cancerous support cells) can shield tumors from immune attack—a challenge these models help visualize.
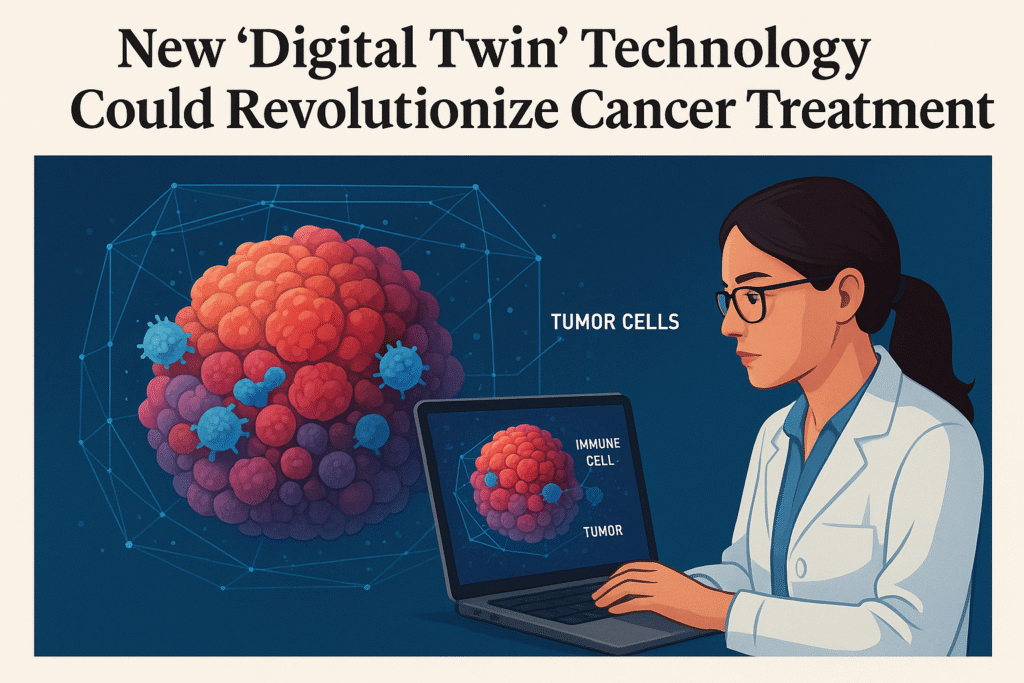
What sets this research apart is its potential for precision medicine. The simulations showed that each virtual “patient” responded differently to treatment, emphasizing the need for personalized cancer therapies.
Dr. Elana Fertig, Director of IGS, described the work as creating a “virtual cell laboratory” where scientists can test hypotheses and predict treatment outcomes without risking patient safety. This approach mirrors weather forecasting models but applies them to biological systems.
Importantly, the new grammar is open-source, allowing researchers worldwide to simulate biological processes—from cancer progression to brain development—using their own data. Collaborators from Johns Hopkins University and Oregon Health Sciences University are already expanding its applications.
“This technology opens doors to digital twins and virtual clinical trials, paving the way for more accurate, patient-specific cancer treatments,” said Dr. Mark T. Gladwin, Dean of UMSOM.
The project received funding from the National Cancer Institute (NCI), National Foundation for Cancer Research, and several other organizations. Ongoing efforts aim to integrate this technology further into cancer research and clinical practice.
Stay tuned to nichesystema.com for more such updates!